Retina

The Retinal specialists at the Eye Center of the North Shore provide comprehensive management of both medical and surgical diseases that affect the retina and vitreous. We use state-of-the-art diagnostic tools, lasers, and surgical procedures to aid in diagnosis and treatment. The retinal diseases they treat include macular degeneration, diabetic retinopathy, and other vascular diseases.
Retinal Disease Educational Videos
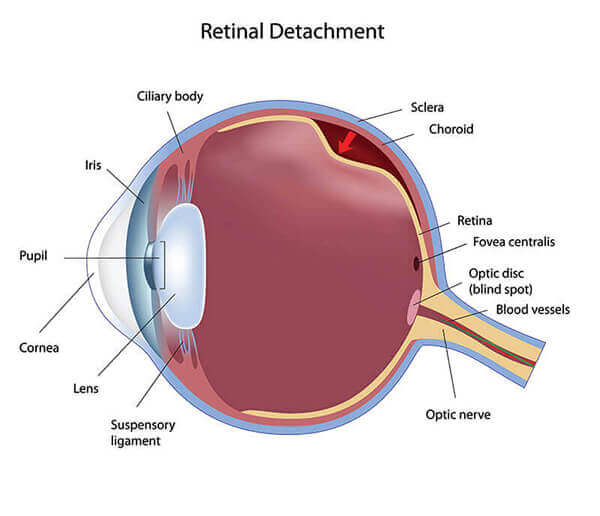
What is a Retinal Detachment?
Definition
The retina is a light-sensitive tissue lining the back of the eye responsible for sending visual signals to the brain via the optic nerve. A healthy and attached retina is crucial to maintaining sight. If the retina pulls away or detaches from its normal position, this can lead to loss of vision.
What Causes a Retinal Detachment?
A retinal detachment can occur at any age without cause. There are certain factors that can increase one’s risk of having a retinal detachment. These include being highly nearsighted, recent eye surgery, trauma, a history of prior retinal detachment, a positive family history of retinal detachments, and disorders/defects of the retina such as lattice degeneration.
What Are the Symptoms of Retinal Detachment?
The onset of a retinal detachment may be heralded by an increased number of cobweb-like floaters in one’s vision and/or flashing lights in the periphery. Depending on the extent of retinal detachment, the patient may experience no change in vision, a partial loss of visual field or an overall decline in vision. This total decline in vision often gives the patient a feeling that a curtain has been pulled over their eyes.
Retinal Detachment Treatment
Treatment depends upon the extent of retinal detachment. Often times, laser surgery is used to weld the retina back into its place if the detachment is limited. A more extensive detachment may be amenable to an in-the-office procedure called cryopexy, where a freezing treatment is applied to the areas of retinal detachment. A gas bubble is also injected into the eye to help push the retina back into position.
Some retinal detachments require the patient to undergo surgery in a controlled operating room. A vitrectomy is one type of such surgery. It involves creating small portals into the eye to remove the existing vitreous jelly and replace it with gas. This gas pushes the retina back against the wall of the eye. This surgery also requires laser or cryopexy to weld or freeze the retina back into place.
A scleral buckle is the second type of procedure used to treat retinal detachments. A synthetic band is used to encircle the eye from the outside bringing the wall of the eye in closer proximity to the detached retina.
Based on the eye exam findings, your ophthalmologist will perform the procedure best suited to you. Retinal detachment surgery has a fairly high success rate when caught in a timely fashion. However, the final outcome can be unpredictable and may require multiple surgical attempts.
What is Diabetic Retinopathy?
Definition
Anyone who has diabetes is at risk of developing diabetic retinopathy. The longer someone lives with diabetes, the greater the potential damage to the retina portion of the eye. Diabetic retinopathy is a condition of diabetes that is caused by changes to the blood vessels in the back of the eye. When blood vessels in the retina are damaged they may leak fluid or blood. This can lead to visual blurring or distortion of the images that the retina sends to the brain. In more advanced stages the disease can lead to blindness. Diabetic retinopathy is the leading cause of blindness for American adults.
Cause and Symptoms

At the initial onset of this condition, there may be little or no symptoms whatsoever. This is precisely why regular eye exams are critical for diabetics. Further progression of the disease can cause visual loss in multiple ways. Patients in the early stages of the disease are categorized as having nonproliferative diabetic retinopathy (NPDR). The retina shows evidence of mild bleeding, retinal swelling, and microaneurysmal changes to the blood vessels. In this stage of the disease, a decline in vision occurs if there is leakage of fluid into the center of vision, also known as macular edema. The more advanced stage of the disease is called proliferative diabetic retinopathy (PDR). In PDR there is a proliferation of abnormal blood vessels. They grow in the retina and can sometimes extend into the jelly substance filling the back of the eye also known as the vitreous. These blood vessels are quite fragile and can easily leak blood into the retina or vitreous leading to a decline in vision. Oftentimes patients will notice floaters or streaks of blood in their vision as a result of bleeding into the vitreous. Retinal detachments may develop as a result of scar tissue formation triggered by the growth of new blood vessels.
Epidemiology
If you are one of many untreated diabetics you are 25 times more likely to develop diabetic retinopathy. According to the American Academy of Ophthalmology, about 80% of people who have diabetes develop some kind of damage to their retina.
Treatment
With diabetes, close management of the disease is the best form of treatment. Keeping tight control over one’s blood sugar levels have been known to delay the onset and progression of diabetic retinopathy. In patients who develop macular edema, laser treatment to the areas of retinal swelling can help increase fluid resorption. In patients who have proliferative diabetic retinopathy, performing scatter laser treatment can help shrink abnormal blood vessels. In patients with bleeding into the vitreous or a retinal detachment, vitrectomy surgery is required to remove the blood from the eye and release any scar tissue tugging on the retina. If you are a patient living in the North Shore of Massachusetts and are concerned about being diabetic call us today for a thorough eye exam.
What is Age-Related Macular Degeneration?
Definition
The macula is the central portion of the retina, the light-sensitive tissue that lines the back of the eye, which allows you to appreciate fine detail. Age-related macular degeneration (AMD), is a disease associated with aging that over time destroys this central tissue. There are two forms of this disease process: a dry form and a wet form. Both forms have the end result of causing vision loss.

What Causes Macular Degeneration?
Dry AMD is caused by a slow break down or death of the macula over time. Wet AMD, on the other hand, is caused by the proliferation of abnormal blood vessels at the level of the macula. These blood vessels are fragile and have a tendency to leak blood and fluid. Both processes lead to a blurring of the central vision, but the changes occur more rapidly in wet AMD. The onset of the disease can be accompanied by the development of drusen, yellowish deposits in the back of the retina. The presence of drusen alone does not translate into macular degeneration. Studies have shown that there is an increased risk of developing macular degeneration correlating with increased size or number of such deposits.
Risk factors for macular degeneration include being Caucasian, smoking, having a family history of the disease, and female gender among many others.
What Are the Symptoms of Macular Degeneration?
The early symptoms for patients with dry AMD are a blurring of vision. Patients most often have a hard time recognizing people and objects. They often require more light and magnification when reading or performing other tasks. With wet AMD, the earliest symptoms involve a distortion of images. Often times, straight lines can appear crooked. Over time, this can progress to a loss of central vision.

Macular Degeneration Treatment
No form of treatment exists for dry AMD. Studies have shown that taking a special formulation of antioxidants and zinc can reduce the risk of the disease progression to an advanced stage.
Wet AMD, on the other hand, does have many treatment options available. This includes laser treatment aimed at destroying the abnormal blood vessels to receiving injections of medications in the eye. Medications have been developed to block the production of abnormal blood vessels and promote resorption of blood and fluid that has already leaked into the macula. Patients commonly require multiple injections in order to have a positive effect. If despite treatment patients continue to have poor vision, a low vision evaluation is recommended. The patient can be introduced to a variety of visual aids that can improve their quality of life.
On a daily basis, patients are encouraged to monitor their vision using an Amsler grid. This is a grid analogous to a checkerboard that allows you to detect any missing areas or visual distortions. If any changes are noted on the Amsler grid, you should immediately get in touch with your ophthalmologist to schedule an exam.
What Are Flashes and Floaters?
Definition
Flashes and floaters are visual phenomena associated with changes occurring to the back compartment of the eye. Floaters are small dark shapes that appear in your field of vision. Often times they look like squiggly lines, specks or cobwebs that move with eye movement. They are most apparent against light background colors or in well-lit areas. Flashing lights can be described as thunderbolts, a spark or an arc of light occurring in the periphery of vision.
What Are the Symptoms of Flashes and Floaters?
While flashing lights and floaters become more common with age you should alert your ophthalmologist if you notice the following:
- a large new floater or a shower of floaters
- sudden onset of flashing lights
- a loss of vision in the periphery
What Causes Flashes and Floaters?
Floaters occur when the vitreous, the jelly in the back of the eye, degenerates or shrinks. As the vitreous shrinks, strands form that cast a shadow upon the retina. While these strands look like they are in front of your eye, they are actually inside your eye. The vitreous tends to degenerate with age. This process is also accelerated in people who are very nearsighted or have incurred ocular trauma among many other causes. A complete breakdown of the vitreous and separation from its attachment to the retina can cause a posterior vitreous detachment. This appears as a large ring-like floater. Approximately 15% of posterior vitreous detachments are associated with an underlying retinal detachment.
Flashes occur when the vitreous is bouncing against or tugging on the retina. This mechanical action translates as a flash of light by the retina. Vitreous degeneration and retinal detachment can both trigger symptoms of flashing lights.
Since a retinal detachment is a serious vision-threatening consequence that can be associated with symptoms of flashing lights and floaters, an examination by an ophthalmologist is recommended.
Treatment
There is no treatment for floaters. Over time, these strands may settle at the bottom of the eye but never fully go away. In rare cases, some surgeons may perform a vitrectomy to remove the vitreous of the eye and replace it with a saline solution. This is rarely recommended.
If flashing lights are associated with normal aging, no treatments are available. If the symptoms of flashing lights or floaters are associated with an underlying retinal tear or detachment then further options are available. These include laser treatment or surgical repair of the retina.
